Home » Conditions » Intimate area » Urinary incontinence
Urinary incontinence is the involuntary loss of urine. It is a common condition that often causes embarrassment and distress, leading many women to remain silent about it. Feelings of guilt, anxiety, and even depression can develop. Contrary to popular belief, this issue does not only affect elderly women. Stress urinary incontinence is frequently observed in women between the ages of forty and fifty.

Urinary incontinence is caused by an increase in intra-bladder pressure that overcomes the bladder sphincter, which then allows urine to pass. This increase may be caused by bladder hyperactivity or by an increase in abdominal pressure.
The main causes of stress urinary incontinence are :
There are contributing factors that increase abdominal pressure or weaken the pelvic floor muscles : constipation, excess weight, pregnancy, sedentary lifestyle, and a history of pelvic or gynecological surgery.
The symptoms of stress urinary incontinence have an impact on quality of life. This condition can lead to social discomfort, affect self-confidence and limit participation in certain activities.
The symptoms are :

There are three main types of urinary incontinence :
Stress urinary incontinence is the most common, affecting nearly half of all women. Mixed incontinence ranks second in prevalence, followed by urge incontinence.
There are several solutions to treat or prevent the worsening of stress urinary incontinence.
Simple advice can improve this condition. It involves eliminating contributing factors : constipation, excess weight, smoking, sedentary lifestyle, and factors that increase abdominal pressure (carrying heavy loads, intense efforts…).
Perineal rehabilitation plays a fundamental role in managing this condition. The goal is to strengthen the pelvic floor and to control the perineal muscles.

Laser treatment is a non-invasive and effective method for treating stress urinary incontinence. This treatment uses laser technology to gently heat the tissues of the pelvic floor, thereby stimulating collagen production and strengthening the supporting structures.
This procedure is effective for mild and moderate stress urinary incontinence.
In women suffering from stress urinary incontinence, the metabolism of the connective tissue of the vaginal mucosa is altered, causing a decrease in the production of collagen necessary for the supporting function.
The vaginal laser stimulates collagen synthesis, improves the trophicity (thickness and quality) of the vaginal mucosa, its vascularization and its elasticity.
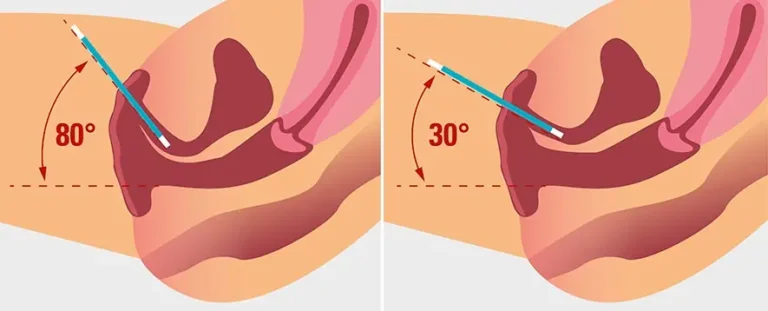
The session consists of several steps.
Intimate laser treatment is an innovative, non-invasive solution appreciated for its effectiveness on vaginal laxity, intimate dryness and stress urinary leakage.
The advantages of laser treatment are :
The results are quite fast. One month after the first session, leakage is reduced. The optimal result is obtained four to six months after the session.
The results are :
Depending on the severity of the condition, one session may be enough to stop the leakage. However, Dr Romano recommends completing the three sessions planned in the protocol to stabilise the result.
A maintenance session every one or two years should be performed.
Urinary incontinence should not prevent physical activity. However, it is important to choose exercises that minimize pressure on the pelvic floor to avoid worsening symptoms.
Recommended sports and activities
Sports to avoid
The treatment of mild to moderate urinary incontinence with laser is a non-invasive solution that has now become an integral part of the therapeutic arsenal in intimate medicine. For patients wishing to undergo it, the price of one laser session for urinary incontinence is set at 600 CHF.
The number of sessions required varies according to the degree of urinary discomfort, age, hormonal context and tissue response. In most cases, during the first year, a series of 2 to 3 sessions, spaced a few months apart, is proposed to achieve significant and long-lasting improvement. A personalised treatment plan is systematically established after evaluation.
The overall cost of laser treatment for urinary incontinence is therefore directly linked to the number of sessions performed. However, the fee remains clear, with no unexpected additional costs, and is the subject of a detailed quote before any treatment.
Patient reviews from those who have chosen laser treatment for stress urinary incontinence are positive, demonstrating the effectiveness of this non-invasive method.
Many women describe a significant reduction in urinary leakage after just one session.
The procedure is also appreciated because it is simple, quick and painless, requiring neither anesthesia nor recovery time.
The laser stimulates collagen production by gently heating the pelvic floor tissues, improving their firmness and support function.
The number of sessions required depends on the severity of the incontinence. In general, 2 to 3 sessions are recommended for optimum results.
Laser treatment offers fast, long-lasting results without the risks and recovery times associated with more invasive procedures.
Patients can expect a significant reduction in bladder weakness, improved quality of life and increased self-confidence.
Most patients feel a slight warmth during the procedure, but there is no pain.
Side-effects are minor and transitory: sensation of heat, slight loss of blood.
Healthy women with symptoms of mild to moderate stress urinary incontinence who want a non-invasive solution are good candidates for this treatment. An initial consultation with a doctor will confirm patients' eligibility.
For urge incontinence, anticholinergics such as oxybutynin are often used. For stress incontinence, there is no specific medication.
Yes, urinary incontinence can be treated with medications, surgical interventions, pelvic floor strengthening exercises or behavioral therapies.
The griffonia root and pumpkin seed are known for managing the symptoms of urinary incontinence.
Chamomile tea is renowned for its soothing properties and can help reduce the frequency of urination.
The essential oil of cypress is often used for its astringent and toning properties.
Kegel exercises are the most recommended.
Common homeopathic remedies are Equisetum and Belladonna.
Regular Kegel exercises help to strengthen and tighten the muscles of the perineum.
Kegel exercises and the use of devices such as vaginal cones can be effective in strengthening the perineum after the age of 60.
Yes, regular walking can help maintain good muscle tone, including that of the perineum.
Geisha balls help strengthen the pelvic floor muscles, improving urinary control and bladder tone.
Electro-stimulators for the pelvic floor.
Pilates and yoga are excellent for strengthening the pelvic floor.
Rehabilitation can be achieved through daily Kegel exercises and the use of biofeedback devices.
Multiple births, intense exertion and inappropriate sporting activities can weaken the perineum.
The causes are pregnancy, childbirth, age, menopause, obesity, and certain chronic diseases.
Consult a doctor if urinary leakage is frequent, affects your quality of life or is accompanied by other symptoms.
Illnesses such as diabetes, urinary tract infections and neurological disorders can cause bladder weakness.
Age, sex (more frequent in women), family history, smoking and certain physical activities are risk factors.
Bladder weakness can occur at any age, but is more common after the age of 40, especially in women after the menopause.
The examinations are a urine analysis, an ultrasound, a cystoscopy and urodynamic tests to evaluate the function of the bladder and the urethra.
Yes, stress can exacerbate the symptoms of an overactive bladder and cause urinary leakage.
Spicy foods, citrus fruits, chocolate and artificial sweeteners can irritate the bladder.
Yes, caffeine is a bladder irritant and can worsen the symptoms of urinary incontinence.